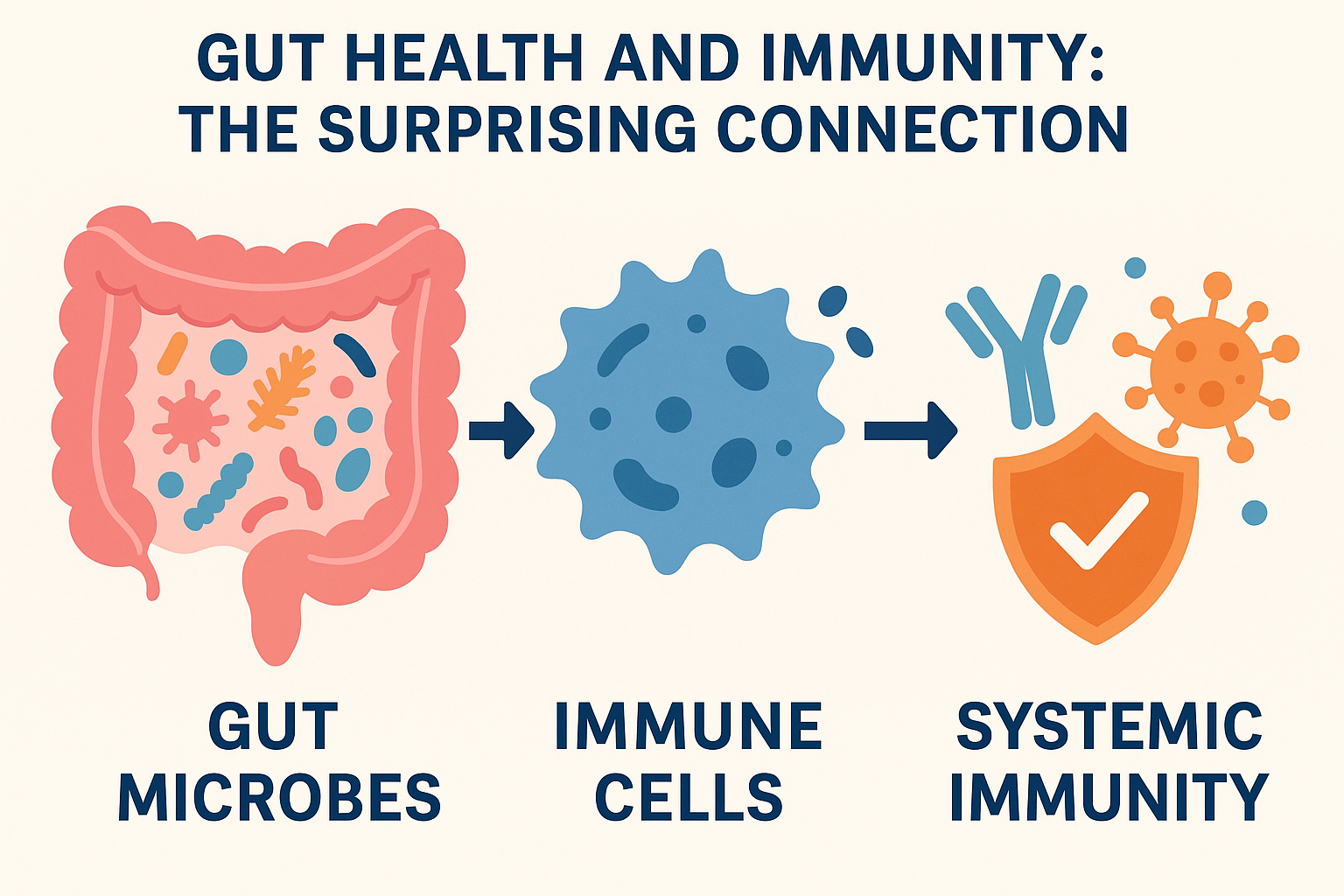
Gut Health and Immunity: The Surprising Connection

Introduction
For decades, the immune system was considered a self-sufficient defense force, separate from other body systems. Today, modern science has revealed a fascinating truth: the gut and its trillions of resident microbes are deeply intertwined with immune health. Nearly 70% of immune cells reside in the gut-associated lymphoid tissue (GALT), making the intestine not just a digestive organ but a central hub of immunity. Understanding this relationship allows us to approach health in a more integrated and preventive way.
General Readers
Think of your gut as a bustling city filled with trillions of friendly citizens—bacteria, fungi, and other microbes—working together to keep you healthy. These microbes break down food, produce vitamins, and even send messages to your immune system. When the balance of this community is disturbed (through poor diet, stress, or excessive antibiotics), harmful bacteria can grow and weaken your immunity. This makes you more prone to infections, allergies, and even autoimmune diseases.
In simple terms, a healthy gut equals a stronger shield against illnesses. Eating fiber-rich foods, fermented products like yogurt, and avoiding unnecessary antibiotics are simple steps everyone can take to protect this shield.
Medical Students
The gut–immune axis is a dynamic interface where epithelial barriers, commensal microbes, and immune cells interact constantly. GALT comprises Peyer’s patches, isolated lymphoid follicles, and mesenteric lymph nodes that sample antigens and regulate immune responses. Pattern recognition receptors (PRRs) such as Toll-like receptors (TLRs) recognize microbial-associated molecular patterns, stimulating cytokine production.
Commensal bacteria promote regulatory T-cell (Treg) differentiation, maintaining immune tolerance, while dysbiosis shifts the balance toward pro-inflammatory Th17 responses. This explains the link between altered gut flora and disorders like inflammatory bowel disease (IBD), allergies, and metabolic syndrome.
Young Doctors
Clinically, gut health should be considered a major determinant of immunity in both preventive and therapeutic practice. Antibiotic overuse, proton pump inhibitors, and highly processed diets often disrupt the gut microbiome. Emerging evidence connects dysbiosis not only with gastrointestinal illnesses but also with systemic conditions such as obesity, diabetes, rheumatoid arthritis, and even neurodegenerative diseases.
In practice, physicians should integrate gut-focused strategies into patient counseling—emphasizing dietary fiber, probiotic supplementation where indicated, and minimizing unnecessary antibiotic prescriptions. Recognizing early signs of gut-immune imbalance, such as recurrent infections, unexplained fatigue, or persistent gastrointestinal complaints, can lead to more holistic care.
General Practitioners
For the family physician, the gut-immune connection offers both a preventive and therapeutic window. Many patients present with vague, non-specific complaints—bloating, fatigue, recurrent infections, or skin rashes. Instead of addressing these in isolation, a GP should assess lifestyle, diet, and medication history. Counseling patients on healthy eating patterns (fruits, vegetables, legumes, whole grains), encouraging fermented foods, and discouraging self-prescription of antibiotics are small but impactful interventions.
Additionally, patients with chronic illnesses like diabetes or autoimmune diseases benefit significantly when their gut health is optimized, as it may reduce inflammatory burden and improve treatment outcomes.
When to See the Doctor
While mild digestive issues can often be managed with lifestyle changes, medical attention is essential if:
• Digestive problems persist beyond two weeks.
• There is unexplained weight loss, blood in stools, or persistent abdominal pain.
• Recurrent infections, allergies, or autoimmune symptoms develop.
• Chronic fatigue or brain fog accompanies gut complaints.
These signs may indicate a deeper imbalance requiring proper investigation and management.
Conclusion
The gut is more than a digestive organ—it is the training ground and command center for immunity. From everyday colds to chronic inflammatory conditions, the state of our gut microbiome profoundly influences our body’s defense system. For patients, simple lifestyle modifications can strengthen immunity. For physicians, understanding the gut–immune axis opens doors to preventive medicine, integrative therapy, and improved long-term outcomes.
A healthy gut is not just about digestion—it is about protection, resilience, and whole-body wellness.