Kidneys: The Unsung Filters That Keep You Alive

By Dr. MTK
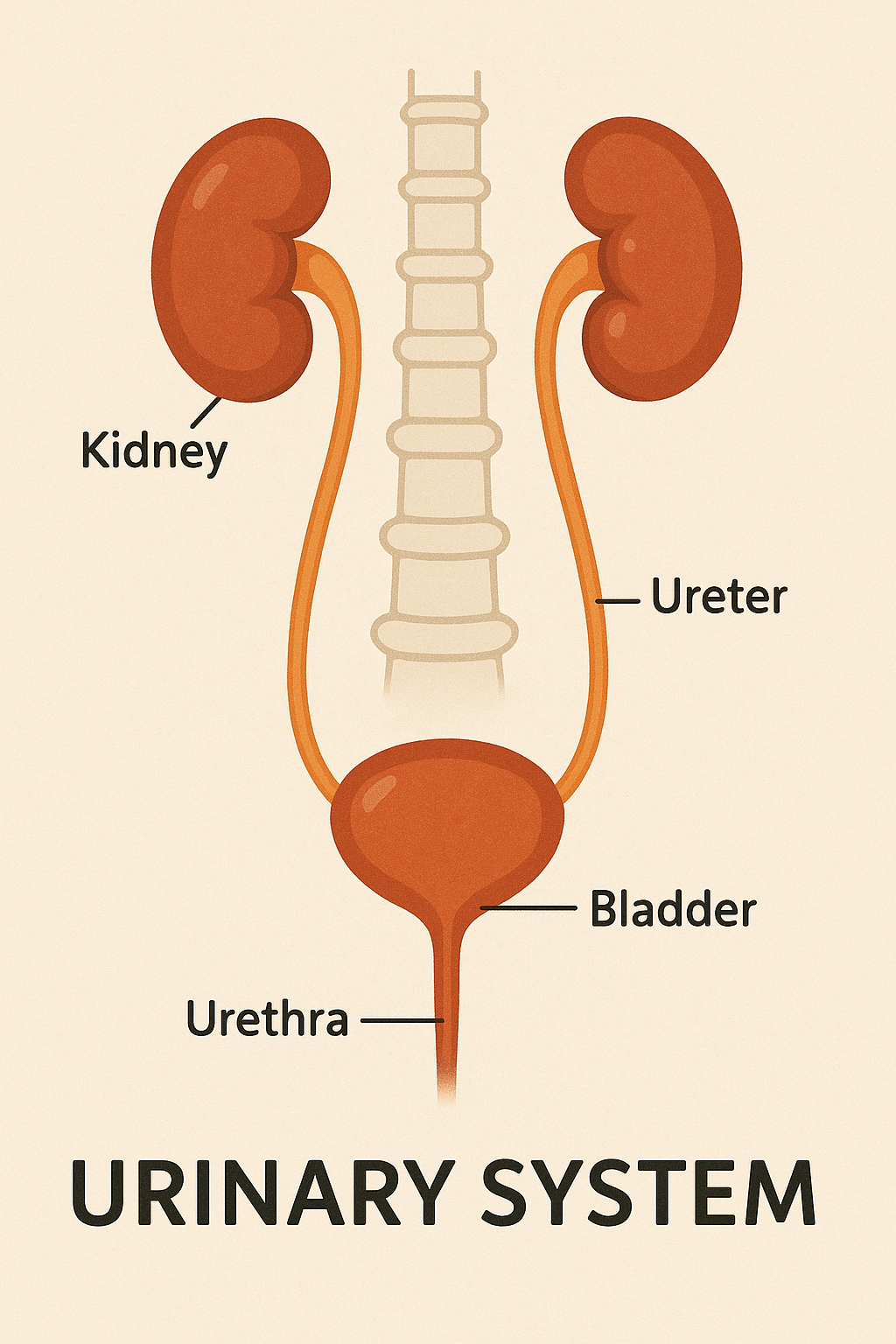
Your kidneys are working right now — quietly, continuously, and without complaint — to keep you alive. Each about the size of a fist, tucked under your ribcage towards your back, these bean-shaped organs filter roughly 50 gallons of blood every single day. They remove waste, balance electrolytes, regulate blood pressure, and even influence your bone strength and red blood cell production. Despite this incredible workload, most people rarely give their kidneys a second thought — until something goes wrong.
From a physician’s point of view, I often see patients who come with vague symptoms — fatigue, loss of appetite, swelling of the feet, or changes in urine — only to discover their kidneys have been under silent strain for years. The tragedy is that kidney damage is often preventable, yet it is usually detected late because the organs themselves do not complain. They have no pain fibers inside to signal distress until the damage is severe.
The kidneys’ role goes far beyond filtration. They help regulate blood pressure through the renin-angiotensin-aldosterone system, maintain the body’s acid-base balance, and ensure that minerals like sodium, potassium, calcium, and phosphorus remain within precise limits. They also produce erythropoietin, a hormone essential for stimulating the bone marrow to make red blood cells. A decline in kidney function can therefore trigger a cascade — anemia, brittle bones, electrolyte disturbances, and fluid overload.
As a physician, I advise that protecting your kidneys begins with understanding your risk. People with diabetes, hypertension, heart disease, obesity, or a family history of kidney disease should have regular blood (creatinine, eGFR) and urine (protein) tests. Avoiding excessive painkiller use, staying well-hydrated, and keeping blood sugar and blood pressure in control are not mere lifestyle tips — they are life-preserving measures.
I often remind patients: the kidneys will serve you faithfully for decades if you serve them back with care. That means not ignoring early warning signs — foamy urine, ankle swelling, persistent fatigue, or reduced urine output — and seeking medical evaluation promptly. With timely detection, many kidney conditions can be stabilized, and in some cases, reversed.
The kidneys may be silent workers, but their absence speaks loudly — dialysis or transplantation becomes the only path forward when they fail. Treat them as you would any vital organ, because without their constant vigilance, life itself would grind to a toxic halt.
1. For Medical Students
Kidneys: The Unsung Filters That Keep You Alive
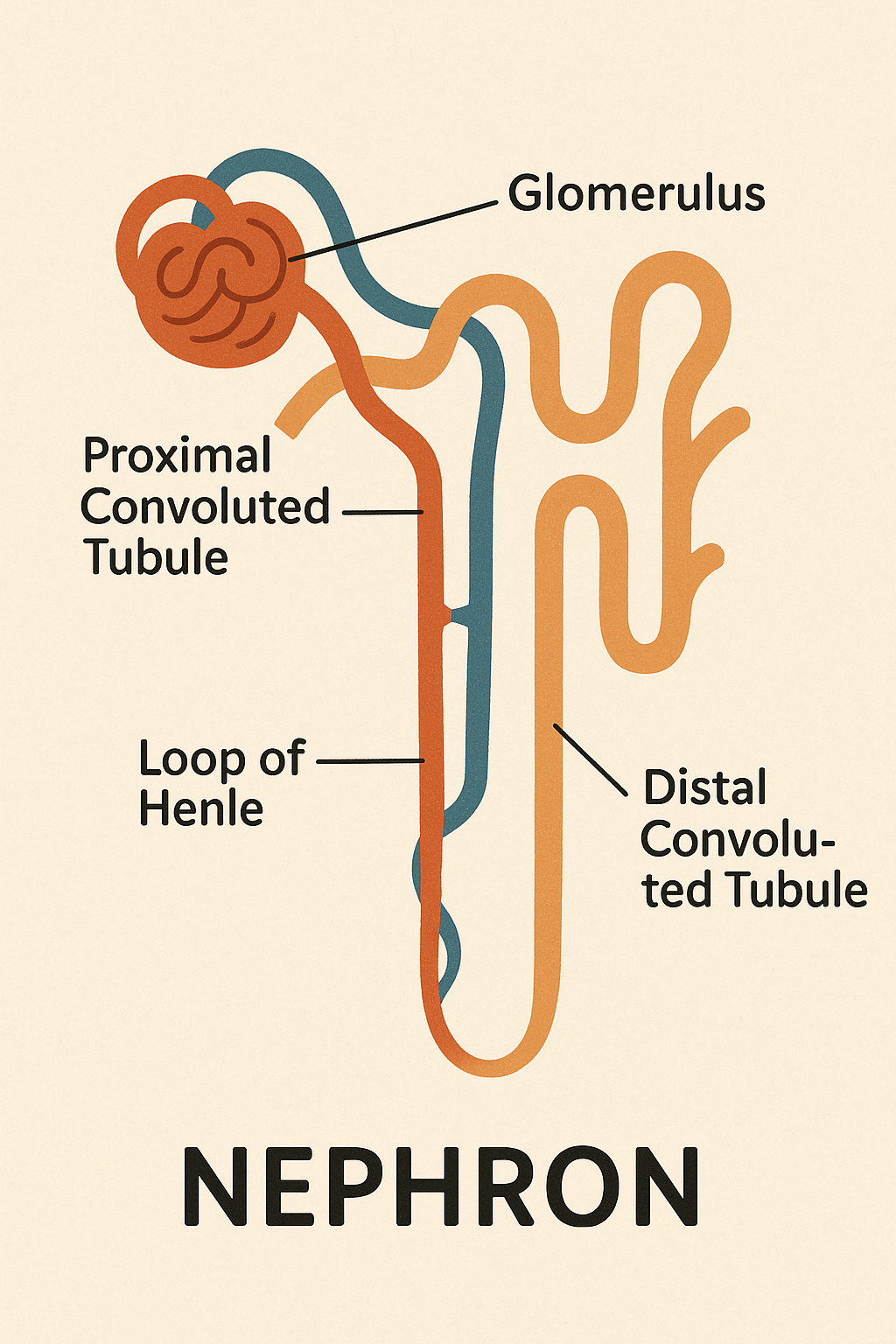
The kidneys, paired retroperitoneal organs located at the T12–L3 vertebral level, perform a daily filtration miracle. Each kidney contains roughly one million nephrons — the functional units where filtration, reabsorption, secretion, and excretion occur. Through the glomerular filtration barrier, plasma is filtered under hydrostatic pressure, producing about 180 liters of filtrate daily, of which more than 99% is reabsorbed.
Physiologically, the kidneys are responsible for:
• Excretion of nitrogenous waste (urea, creatinine, uric acid)
• Electrolyte homeostasis (Na⁺, K⁺, Ca²⁺, PO₄³⁻)
• Acid–base balance via bicarbonate reclamation and hydrogen ion excretion
• Blood pressure regulation through the renin–angiotensin–aldosterone system
• Erythropoiesis regulation via erythropoietin secretion
• Bone health via activation of vitamin D (calcitriol)
Clinically, chronic kidney disease (CKD) is often silent until advanced stages. Early detection depends on serum creatinine, estimated GFR, and urine albumin-to-creatinine ratio. Common etiologies include diabetic nephropathy, hypertensive nephrosclerosis, and glomerulonephritis.
Key takeaway for students: Integrate pathophysiology with patient symptoms. For example, peripheral edema in CKD relates to sodium and water retention; anemia results from reduced erythropoietin production; metabolic acidosis arises from impaired acid excretion.
2. For Young Doctors
Kidneys: The Unsung Filters That Keep You Alive
In clinical practice, the kidneys demand our vigilance precisely because they fail silently. Always maintain a high index of suspicion in high-risk patients — those with diabetes, hypertension, cardiovascular disease, autoimmune disorders, or prolonged NSAID use.
Approach to a Patient with Suspected Renal Dysfunction:
• History — changes in urine volume/character, edema, fatigue, anorexia, flank discomfort, pruritus.
• Examination — blood pressure, pedal edema, pallor, signs of fluid overload, uremic frost (rare, advanced).
Investigations —
• Blood: Creatinine, BUN, electrolytes, bicarbonate, eGFR
• Urine: Routine exam, protein quantification, sediment microscopy
• Imaging: Renal ultrasound for size, echotexture, obstruction
• Risk stratification — stage CKD (KDIGO classification) for prognosis and management planning.
Management priorities: Control underlying disease (BP <130/80 mmHg, HbA1c <7%), reduce proteinuria (ACE inhibitors/ARBs), manage anemia, correct electrolyte imbalances, avoid nephrotoxins, vaccinate (hepatitis B, pneumococcal), and prepare for renal replacement therapy if progression occurs.
Key reminder: Never underestimate minor lab deviations — a “slightly raised” creatinine might indicate a 50% reduction in GFR. Early intervention can delay progression by years.
3. For General Practitioners
Kidneys: The Unsung Filters That Keep You Alive
In primary care, the kidneys deserve routine attention, especially in patients over 40 or with comorbidities. Many cases of kidney disease can be detected early — and progression slowed — with vigilant screening.
Practical GP approach:
• Include serum creatinine and urine protein testing in annual checkups for at-risk groups.
• Educate patients on avoiding excessive salt, uncontrolled sugars, overuse of painkillers, and dehydration.
• Monitor blood pressure regularly; aim for <130/80 mmHg in CKD patients.
• Address lifestyle factors — encourage hydration, balanced diet, and regular exercise.
• Be alert to early red flags: persistent ankle swelling, frothy urine, unexplained fatigue, nocturia.
When abnormalities are found, repeat testing within weeks before labeling CKD, and refer to a nephrologist early if:
• eGFR <60 mL/min/1.73 m² and declining
• Persistent proteinuria or hematuria
• Unexplained rapid rise in creatinine
Your role as a GP is twofold — early detection and long-term follow-up. Many patients will never require dialysis if risk factors are addressed aggressively from the start.
When to see the doctor ?
For kidney and urinary system health, you should see a doctor promptly if you notice any of the following:
• Changes in urine — blood in urine, foamy urine, very dark urine, or persistent foul smell
• Swelling — especially in ankles, feet, face, or around the eyes
• Pain — persistent lower back pain (near the flanks) or burning sensation during urination
• Changes in urination pattern — too much, too little, or difficulty urinating
• Unexplained fatigue or weakness — may be due to anemia from reduced kidney function
• High blood pressure — especially if it’s new or poorly controlled
• Recurrent urinary tract infections — or infections accompanied by fever and chills
• Persistent nausea, vomiting, or loss of appetite — possible signs of uremia
• Foamy urine that lasts — indicating possible protein leakage
• Family history — kidney disease, polycystic kidney disease, or chronic hypertension/diabetes
Golden rule as a physician:
If a symptom involves a change in urine, swelling, pain in the urinary tract area, or persistent unexplained fatigue, don’t delay — early testing can prevent years of silent kidney damage.