The Gut–Brain Connection — How the Intestines Influence Mood, Immunity & Hormones
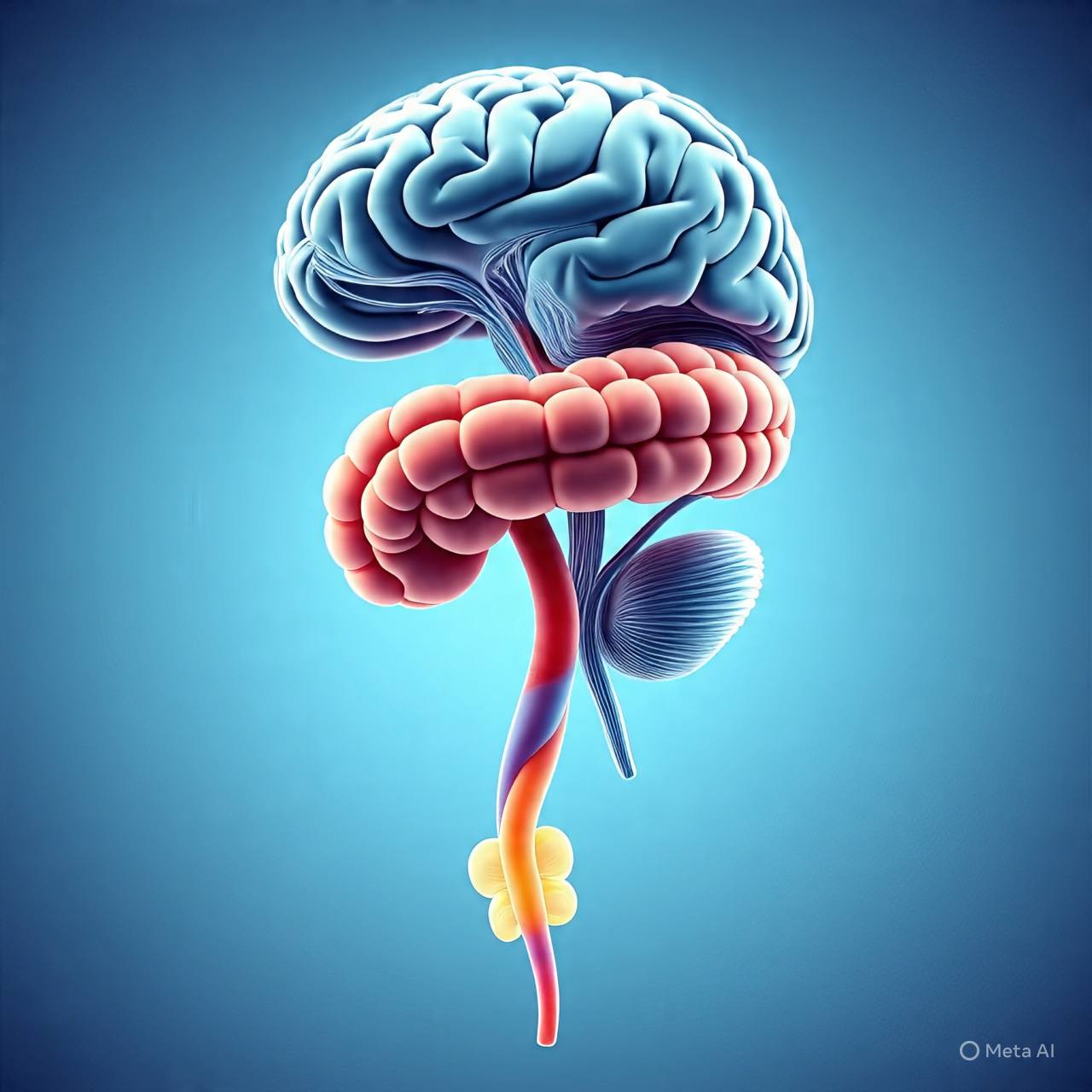

The gut is not just a digestive tube. It is a dynamic communication hub, filled with neurons, hormones, immune cells, microbiota colonies, and neurotransmitters — constantly talking to the brain. This bidirectional messaging system is called the Gut–Brain Axis, and it influences far more than digestion. It affects mood, memory, immunity, inflammation, metabolism, and even the way we respond to stress.
Patients are often surprised when anxiety improves after fixing constipation or when depression eases after improving gut health. The truth is — the intestines and brain are inseparable partners.
General Readers
In simpler words:
Your gut and your mind speak to each other all day long.
When your intestines are healthy, you feel calmer, energetic, focused, and emotionally balanced. When they are inflamed, irritated, or disturbed, the brain often responds with anxiety, fatigue, mood swings, forgetfulness, irritability, and sleep problems.
Signs your gut may be affecting your brain:
• Gas, bloating, constipation or diarrhea
• Mood instability or irritability
• Anxiety, unexplained sadness
• Fatigue even after sleeping
• Sugar cravings and emotional eating
• Skin flare-ups, hair fall, poor immunity
Your gut produces about 90% of the body’s serotonin, the happiness neurotransmitter — so emotional health begins inside the intestines.
Medical Students
Key concepts to understand:
• Gut–Brain Axis involves neural, immune, metabolic and endocrine interaction
• Vagus nerve is the primary physical communication pathway
• Microbiota produce neuroactive compounds (GABA, serotonin precursors)
• Dysbiosis → ↑ inflammatory cytokines → crosses BBB → affects mood/cognition
• Stress increases gut permeability → “leaky gut” → systemic inflammation
• Diet, antibiotics, and sleep regulate microbial diversity
Examiners commonly question:
Understanding gut physiology today is essential for future psychiatry, neurology & internal medicine practice.
Young Doctors
In clinics, patients rarely say “My gut is affecting my brain.”
They present with:
• IBS-like bowel discomfort + panic episodes
• Gastritis + tension headaches
• Bloating + chronic fatigue
• Constipation + brain fog
• Dysbiosis symptoms + insomnia
Treatment approach must be holistic, not symptomatic.
Recommended clinical basics:
• Improve diet before medication escalation
• Encourage sleep hygiene & circadian alignment
• Screen for chronic stress & anxiety patterns
• Replace unnecessary antibiotics with probiotics support
• Educate patients: mind affects gut, gut affects mind
A conversation sometimes works better than a prescription.
General Practitioners
Your role is central. You meet these patients daily.
Key steps for management:
Detailed history — bowel habits, stress, sleep, antibiotics
Evaluate diet (fiber, fermented foods, processed sugar intake)
Start gut-friendly interventions before psychiatric referrals
Rule out red flags: blood in stool, weight loss, nocturnal pain
For persistent IBS, think dysbiosis + vagal imbalance
A patient with depression and persistent abdominal symptoms rarely improves until the gut is treated simultaneously.
Pathophysiology (Simplified but Scientific)
• Microbiome produces neurotransmitters
• Serotonin, dopamine, GABA precursors → mood regulation
• Vagus nerve = communication cable
• Signals travel from intestines to emotional centers of brain
• Inflammation crosses the blood-brain barrier
• Cytokines alter neural firing + emotional processing
• Leaky gut → immune activation → neuroinflammation
• Diet modifies microbial diversity, which directly modifies emotional balance, stress tolerance, appetite, and cognition.
Gut health = Neurological stability.
When to See a Doctor
Seek medical evaluation if you have:
Persistent abdominal pain or bloating
Constipation/diarrhea lasting >4 weeks
Anxiety + gut discomfort together
Sudden change in bowel habits
Blood in stool or unexplained weight loss
Sleep disturbance with digestive symptoms
Fatigue despite normal labs
Early intervention prevents chronic gut-brain dysregulation.
Your gut is a second brain — producing hormones, neurotransmitters and immune signals that shape how you think, feel and function. Healing the gut is often the first step toward emotional balance, mental clarity, and whole-body well-being.
If the gut is calm, the mind follows.
Dos and Don’ts
DO
✔ High-fiber diet, vegetables, whole grains
✔ Fermented foods (yogurt, kefir, kimchi)
✔ Daily physical activity
✔ Adequate hydration
✔ 7–8 hours of deep sleep
✔ Mindful slow eating
✔ Manage stress through breathing & sunlight exposure
DON’T
✘ Overuse antibiotics
✘ Rely on antacids for long periods
✘ Skip meals or eat late-night snacks
✘ Excess refined sugar & processed foods
✘ Ignore persistent gut symptoms
✘ Neglect sleep — it controls the microbiome
FAQs
Q1. Can treating the gut improve anxiety or depression?
Yes. Many patients notice emotional stability once digestion improves.
Q2. Are probiotics necessary for everyone?
Not always. Natural fermented foods are often enough unless dysbiosis is severe.
Q3. Why do I feel tired even when my labs are normal?
Inflamed gut + poor absorption + microbial imbalance may reduce energy availability.
Q4. Can gut issues cause sleep disturbance?
Yes — cortisol fluctuations, serotonin imbalance, and inflammation all affect sleep.
Q5. What is the fastest way to improve gut health?
Fiber, hydration, sleep, sunlight, stress reduction and consistent meals.

By Dr. Mohammed Tanweer Khan
A Proactive/Holistic Physician
Founder of WithinTheBody.com